In early 2025, the Trump administration has enacted sweeping cuts to U.S. foreign aid, profoundly impacting health systems across Africa. Through Executive Order 14169, a 90-day pause on all U.S. foreign development assistance programs was initiated, leading to the suspension of critical health services and the dismantling of long-standing support structures.
The consequences were immediate and severe. In South Africa, where over 8 million people live with HIV, the halt in funding disrupted antiretroviral treatment programs, jeopardizing the health of millions. In Kenya, the cessation of aid led to the closure of clinics and the loss of thousands of healthcare jobs, leaving vulnerable populations without access to essential services.
The cuts extended beyond HIV/AIDS programs. Malaria prevention initiatives, tuberculosis treatment, maternal and child health services, and nutrition programs faced significant setbacks. The abrupt withdrawal of funding forced organizations like UNICEF and Save the Children to scale back operations, affecting millions of women and children across the continent.
Moreover, the dismantling of USAID and the suspension of contributions to the World Health Organization and the Global Fund to Fight AIDS, Tuberculosis and Malaria further strained Africa's health infrastructure. These organizations play a pivotal role in disease surveillance, outbreak response, and the provision of life-saving medications.
The 2025 funding cuts serve as a stark reminder of the volatility of donor-dependent health systems. To build resilience and ensure continuity of care, there is an urgent need to explore self-sustaining models that leverage local resources and partnerships. Investing in digital infrastructure, fostering public-private collaborations, and enhancing domestic funding mechanisms are critical steps toward achieving health system autonomy and safeguarding against future disruptions.
Why “Sustainability” Efforts Have Fallen Short
Donors and implementing partners have long recognized the risks of building digital health tools that can't outlive their funding cycles. In response, many have attempted to "bake in" sustainability through handover plans, capacity-building efforts, local hosting, and government co-ownership strategies. In theory, these are sound ideas. But in practice, they rarely stick.
Handover plans often assume that ministries of health can absorb new costs and responsibilities once a project ends when in reality, digital health rarely makes it into national budgets. Capacity-building focuses on training individuals but not the institutions or business models needed to keep systems alive. Local hosting shifts the technical burden to government IT teams, who are often under-resourced and already overstretched. And co-ownership models tend to blur accountability, resulting in platforms that fall into disuse once the original funder exits.
Even the most well-intentioned sustainability efforts have failed to address the core issue: there is no durable funding mechanism tied to the value the system creates. As a result, countries across Africa are littered with abandoned digital platforms, once-promising lab systems that worked during pilot phases but slowly deteriorated after the grant expired. Others still run, technically speaking, but with outdated data, no maintenance, and no meaningful use.
There is a need for a sustainability model that can stand on its own, one that doesn’t depend on goodwill, but on real, recurring contributions from those who rely on the platform to run their businesses or deliver their services.
A Digital Lab Platform That Funds Itself
If past attempts at sustainability have taught us anything, it’s that goodwill and handover plans are not enough. A truly resilient lab platform needs more than training manuals and capacity building, it needs a business model beyond the donor.
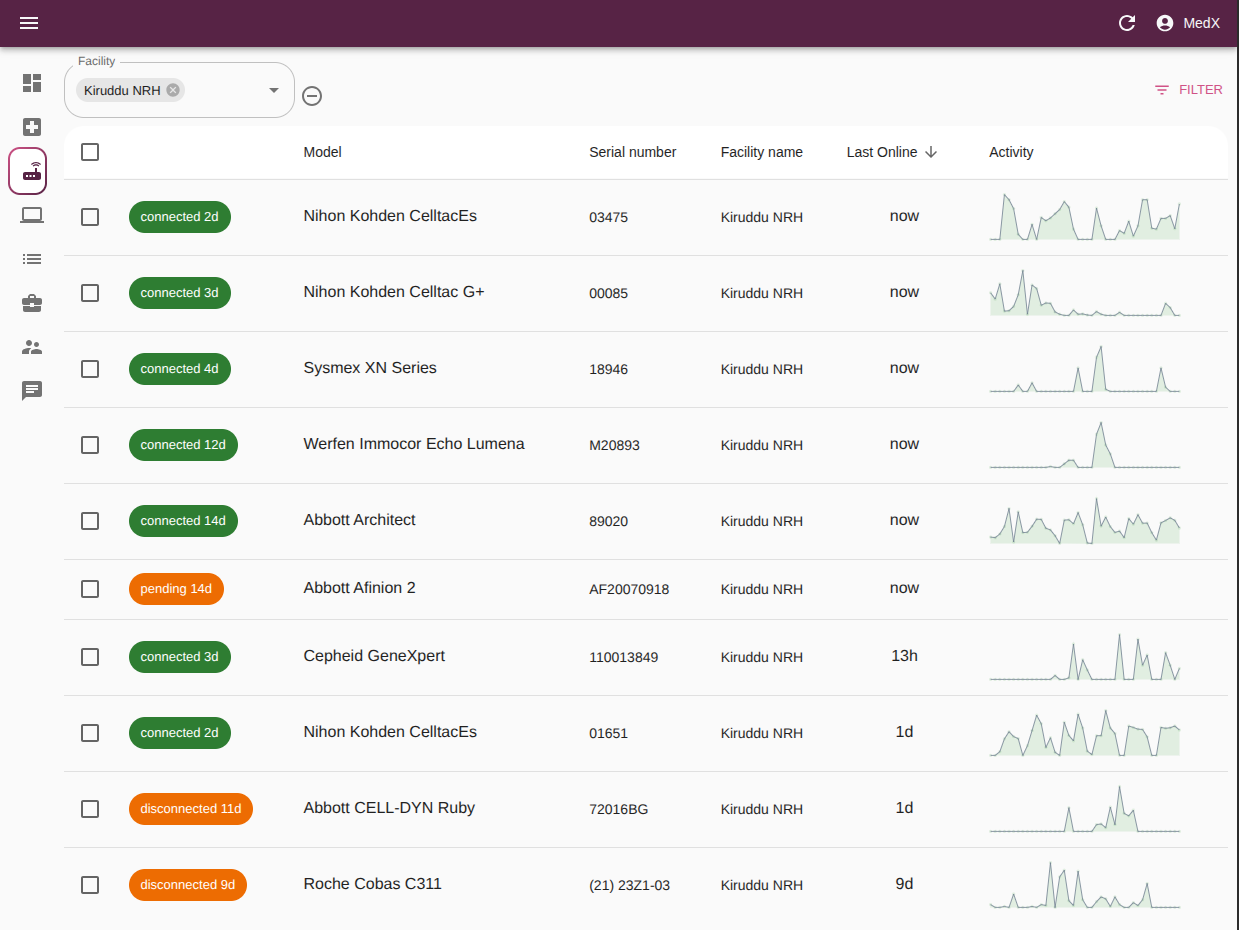
We propose a new kind of national lab system: one that not only supports diagnostics but actively sustains itself through the value it creates for those who rely on it commercially. At its core, the platform provides a full suite of digital lab infrastructure; a shared Laboratory Information Management System (LIMS), equipment monitoring and uptime tracking, referral coordination between labs, analytics dashboards, and seamless integrations with health programs and supply chains.
The businesses who benefit most from well-run labs; equipment vendors, private labs, diagnostic OEMs, and others pay modest recurring fees in exchange for the operational efficiency, insights, and revenue opportunities the platform unlocks. The model is designed to:
- Keep digital infrastructure running well beyond initial funding
- Enhance performance and accountability across the diagnostics ecosystem
- Align the interests of government, commercial partners, and funders
The following sections explore commercial actors already embedded in lab systems and how they have every reason to invest in a platform that helps them work better, faster, and smarter.
Equipment Vendors Supplying the Government
In many low- and middle-income countries, the government doesn't directly purchase lab machines outright. Instead, equipment vendors provide devices like hematology analyzers, chemistry machines, or PCR platforms on placement. This means the machines are installed at no upfront cost, with the understanding that the vendor will recoup their investment through consumable sales over time. Those sales are often channeled through centralized government procurement agencies.
Most of these vendors don’t manufacture the equipment themselves. They represent multiple global OEMs, acting as local distribution and support partners. They respond to tenders, engage with Ministries of Health, and are responsible for installation, user training, and maintenance across facilities. Their business depends entirely on the consistent use of their equipment over time.
But that’s where the challenge begins. Once machines are installed, vendors often have no visibility into how they’re being used, if they’re being used at all and how the consumables are distributed by the national procurement agency. They rely on occasional phone calls from lab staff or sporadic field visits. Equipment may sit idle for weeks due to reagent stockouts, power issues, or user errors. By the time a service technician is dispatched, the vendor may have already lost significant reagent revenue.
A centralized lab platform that includes an equipment management portal changes the equation completely. By plugging into the national lab system, vendors gain real-time insights into how their machines are performing across all government facilities. They can see which sites are running optimally, which ones are underperforming, and why. They receive early warnings about maintenance issues or drops in usage. They can plan service visits more efficiently, avoid unnecessary trips, and ensure that their placement agreements remain profitable.
This kind of visibility also strengthens their position in future procurement. Vendors who can demonstrate consistent uptime, rapid issue resolution, and data-backed support are more likely to be favored in tenders. It’s no longer just about supplying equipment, it’s about guaranteeing performance.
For vendors managing multiple OEMs across a country or region, the platform offers a single window into their entire installed fleet. It helps them protect their margins, reduce servicing costs, and increase reagent turnover all while building stronger relationships with public health systems. In short, the platform doesn’t just help them support the government, it helps them become better vendors.
Private Diagnostic Laboratories
Private diagnostic labs especially those in urban and peri-urban areas are a growing part of the healthcare ecosystem. These labs serve a mix of walk-in patients, private hospitals, corporate clients, and insurance schemes. Their success depends on speed, accuracy, and trust, yet many still operate with paper registers or disjointed systems that barely meet regulatory standards.
For these labs, a fully-featured Laboratory Information Management System (LIMS) is no longer a luxury, it’s a necessity. But building one from scratch, or even licensing a commercial solution, is often prohibitively expensive. Most mid-sized labs can't afford dedicated IT teams or enterprise-grade platforms. Instead, they make do with basic spreadsheets, locally built tools, or manual processes that leave room for error and delays.
This is where a national digital lab platform becomes incredibly valuable. By subscribing to a centrally managed LIMS, private labs can access a modern, cloud-based system without the overhead of development, maintenance, or infrastructure. They gain automated test logging, digital result reporting, internal quality checks, and built-in analytics all designed with regulatory compliance in mind.
Beyond the basics, the platform can also help labs grow. Features like SMS notifications, online result delivery, and equipment interfacing, create new ways to serve patients and referring clinicians. Integration with insurance claim systems, government disease reporting, and regional referral networks helps labs stay compliant and visible within the broader health system.
A particularly important opportunity lies in diagnostic referrals. Today, many private labs already refer certain public health tests, such as TB or HIV confirmatory testing, to government reference labs. With the right digital infrastructure, this referral flow can be expanded to include commercial tests as well. Smaller labs could refer low-volume or specialized tests, such as immunoassays, cultures, or molecular diagnostics, to better-equipped government facilities through the platform.
This creates a new source of revenue for public labs, who can charge private labs for processing referred tests. It also generates transaction revenue for the platform itself, which handles the digital ordering, logistics, and result integration. It’s a win-win: the public system earns more, private labs improve their service offering, and the digital backbone sustains itself through real use.
Most importantly, the platform levels the playing field. Smaller labs gain access to the same digital infrastructure as larger players, allowing them to compete fairly on quality and turnaround time. As test volumes grow and standards tighten, digital efficiency becomes a key differentiation.
Diagnostic OEMs
Diagnostic Original Equipment Manufacturers (OEMs) are the global powerhouses behind the platforms used in molecular diagnostics, immunoassay testing, chemistry, hematology, and beyond. In Africa, companies like Roche, Abbott, Cepheid, Beckman Coulter, BioMérieux, Mindray, and Siemens Healthineers are all heavily represented through local distributors and vendors.
These companies have invested heavily in supporting programs like HIV viral load testing, TB diagnostics, COVID-19 PCR, and routine chemistry panels for public hospitals. Their machines are often embedded into national testing algorithms and supported by donors like PEPFAR, the Global Fund, and the World Bank.
Yet once those machines are deployed, most OEMs lose visibility. They rely on vendors for fragmented feedback and depend on sparse post-market surveillance, especially in public labs. They don’t know if the machines are idle due to stockouts, if staff are struggling with operations, or if a site is burning through reagents inefficiently. Without real-time data, it’s hard for them to improve support, iterate on product design, or optimize reagent logistics.
A national digital lab platform with an integrated equipment monitoring layer solves that. It gives OEMs anonymized, aggregate data on how their platforms are performing across facility types, regions, and patient volumes. They can track utilization, identify high- and low-performing sites, and detect patterns that inform better training, design, and support strategies.
For example, Cepheid, the manufacturer of GeneXpert, could use platform data to understand cartridge consumption rates, machine downtime, or error rates across hundreds of GeneXpert units in different districts. Abbott and Roche, with large-scale chemistry and PCR installations, could analyze how reagent consumption correlates with disease burden or seasonality. Mindray, which is rapidly gaining market share in hematology, could refine its support model based on comparative performance data across public labs.
This kind of insight is critical. These companies are under pressure to maintain global standards while responding to local realities. The more they know about how their platforms are being used, the more effectively they can support governments and outcompete rival technologies.
Paying for access to aggregated, ethically managed analytics is a small price compared to the cost of blind spots, idle machines, or misused platforms.
A Smarter Future for Lab Infrastructure
Digitizing labs shouldn’t hinge on the next donor cycle or the goodwill of the moment. Like power grids or telecom towers, it should be built on infrastructure that sustains itself driven by the value it provides to the people and businesses that depend on it.
Governments need oversight and resilience. Vendors need uptime and visibility. Labs need tools that help them grow. OEMs need insights to stay competitive. And patients, whether public or private, deserve reliable results.
At MedX, we’re actively exploring how a self-sustaining digital lab platform could work—not as a theoretical model, but as a practical solution for countries facing the fragility of donor-funded systems. The technology is mature. The incentives are aligned. What’s needed now is a conversation: with policymakers, vendors, labs, funders, and anyone else invested in making health systems work better for the long haul. If you're part of that ecosystem and want to test, shape, or scale this idea, we’d love to hear from you. Let’s explore together what it would take to build a digital lab infrastructure that lasts.